| Question AQ 001 |
| The
patient is a 72 year old white male with ischemic cardiomyopathy, prior
infero-posterior wall myocardial infarction, status-post three-vessel
coronary artery bypass graft surgery, chronic renal failure and a dual
chamber permanent cardiac pacemaker that was implanted 3 years ago. The
patient was admitted because of generalized weakness. The 2-D echocardiogram in the top row (below, right) shows the right ventricle and right atrium, as selected from the 4-chamber view (below, left). The echocardiogram in the bottom row shows another view of the right ventricle and right atrium, clearly demonstrating the highly mobile mass that prolapses through the tricuspid valve. |
4-chamber view of 2-D echocardiogram: 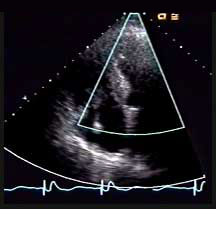
FOR AUDIO: Click the Speaker Icon to "unmute" Audio |
|
FOR AUDIO: Click the Speaker Icon to "unmute" Audio |
| With reference to the echocardiogram of this patient, which one of the following is LEAST likely to be true: |
| Exit |
